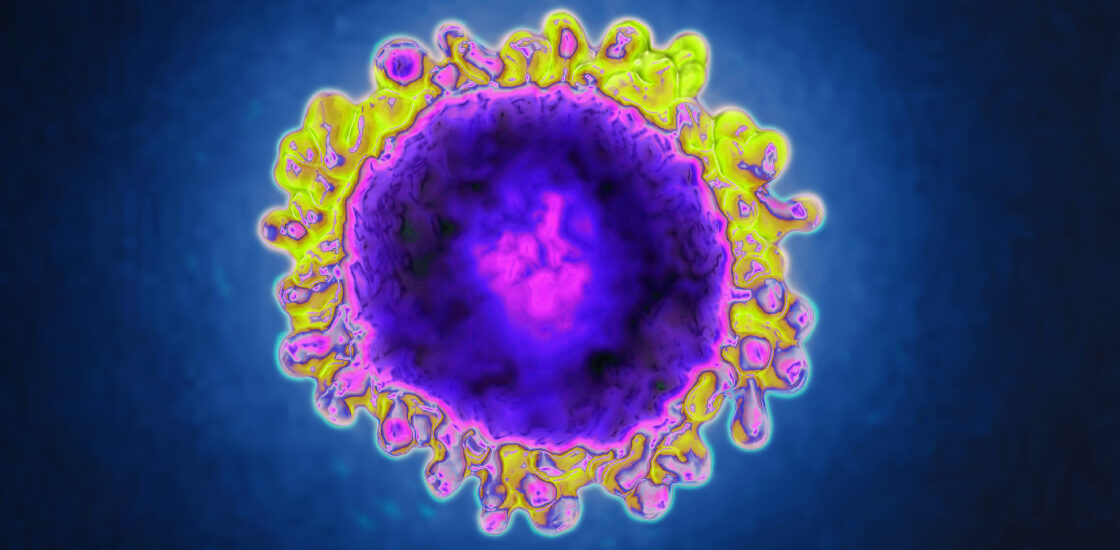
How to protect vulnerable autistic adults during the coronavirus pandemic
Spectrum – Updated for October 2021
Author: Whitney Schott
As the highly contagious Delta variant of the coronavirus challenges efforts to stem the COVID-19 pandemic, it is essential to protect the vulnerable among us — especially adults with autism, intellectual disability or mental health diagnoses. These individuals are at an increased risk of contracting COVID-19 and having severe complications from it because of their living situations and co-occurring health conditions.
Those who live in congregate settings such as group homes or residential facilities may have difficulty maintaining physical distance from other residents or caregivers. Such settings may have outdated ventilation systems that are not sufficiently equipped to filter viral particles. Adults receiving services in their homes may face increased risk of coronavirus exposure from multiple care providers, which could be even higher if there are staff shortages or turnover among health workers. And adults experiencing mobility challenges may find it difficult to access COVID-19 vaccines, tests and medical services.
In addition, adults with autism, intellectual disability or mental health diagnoses often have physical health conditions — including chronic kidney disease, heart conditions, obesity and diabetes — that put them at increased risk of severe disease from COVID-19. We must ensure that these adults are protected with appropriate mitigation measures wherever they may be living or working.
Counting risk factors:
My colleagues and I sought to quantify these individuals’ risks to help inform health policy design related to COVID-19. We examined data from adults who have been enrolled in Medicaid for at least nine consecutive months from 2008 to 2012, including more than 646,000 adults with autism or intellectual disability, as well as a random sample of more than 1 million adults without autism or intellectual disability, about one-third of whom have mental health conditions. We reported our findings in August in Autism.
We found that about half of autistic and non-autistic adults with intellectual disability lived in a residential facility, compared with only 1 percent of the population without any developmental or mental health diagnoses. About one-fifth to one-third of adults with autism or intellectual disability, and one-tenth of adults with mental health diagnoses, regularly received services in the home from outside caregivers, compared with 3 percent of the population without developmental or mental health diagnoses.
The majority of adults with autism, intellectual disability or mental health diagnoses had also been hospitalized during the period of study for conditions that could have been avoided, indicating insufficient access to care. Specifically, 52 percent of autistic adults without intellectual disability, 69 percent of autistic adults with intellectual disability, 67 percent of adults with intellectual disability but not autism, and 65 percent of adults with other mental health diagnoses had had an avoidable hospitalization, compared with 4 percent of adults without these conditions.
In addition, these populations had higher odds of having a condition identified by the U.S. Centers for Disease Control & Prevention as putting one at greater risk of severe illness from COVID-19, including cancer, chronic lung disease, diabetes and severe obesity. Just 16 percent of those without developmental or mental health diagnoses had one or more of these physical health diagnoses, whereas 29 percent of autistic adults without intellectual disability, 32 percent of autistic adults with intellectual disability, 38 percent of adults with intellectual disability but not autism, and 43 percent of adults with other mental health conditions had been diagnosed with at least one of these physical health conditions. Their odds of having one of these conditions remain higher than those in the general Medicaid population after controlling for characteristics such as age, sex, race, ethnicity, Medicaid insurance mechanism, dual eligibility status and state.
Minimizing risks:
Given these vulnerabilities, care providers, advocates and health agencies must work to mitigate risk of COVID-19 among populations with developmental and mental health diagnoses.
For families whose loved one has a developmental or mental health diagnosis, it is important to implement as many mitigation measures as possible to create a buffer against risk. Most importantly, families must make every effort to ensure that their loved one and any eligible individuals around them, including caregivers, service providers, family members and friends, are vaccinated for a baseline level of protection. Previous research suggests that the best way to reach populations with developmental disabilities for vaccination is through a well-known, trusted care provider.
Next, a multi-pronged risk mitigation approach — including vaccination (and boosters when appropriate), mask-wearing, improving ventilation and air filtration, sanitizing and cleaning surfaces, handwashing, avoiding crowds and maintaining physical distancing — is essential. For adults exposed to several caregivers throughout the day or week, a portable HEPA air filter can help to remove viral particles from the air. Family members and care providers of loved ones living in a residential facility can talk to facilities directors about ventilation to ensure that there are six or more air exchanges per hour where their loved one is staying.
Although individuals and families can take action to reduce risk from COVID-19 among adults with developmental and mental health conditions, it is also important that employers, local and state health departments and federal spokespeople help to protect these vulnerable populations through policies encouraging vaccination and through these additional mitigation measures.