What Are the 4 Stages of Rheumatoid Arthritis?
Rheumatoid arthritis (RA) is a chronic autoimmune condition that affects approximately 1.3 million adults in the United States, representing about 0.4% of the adult population, according to the Arthritis Foundation [1]. Understanding the progression of this disease is vital for patients, their families, and healthcare providers in optimizing care and treatment plans. Here, we delve into the four stages of rheumatoid arthritis, shedding light on what are the symptoms of rheumatoid arthritis at each stage and how to manage this condition more effectively.
Stage 1: Early Stage
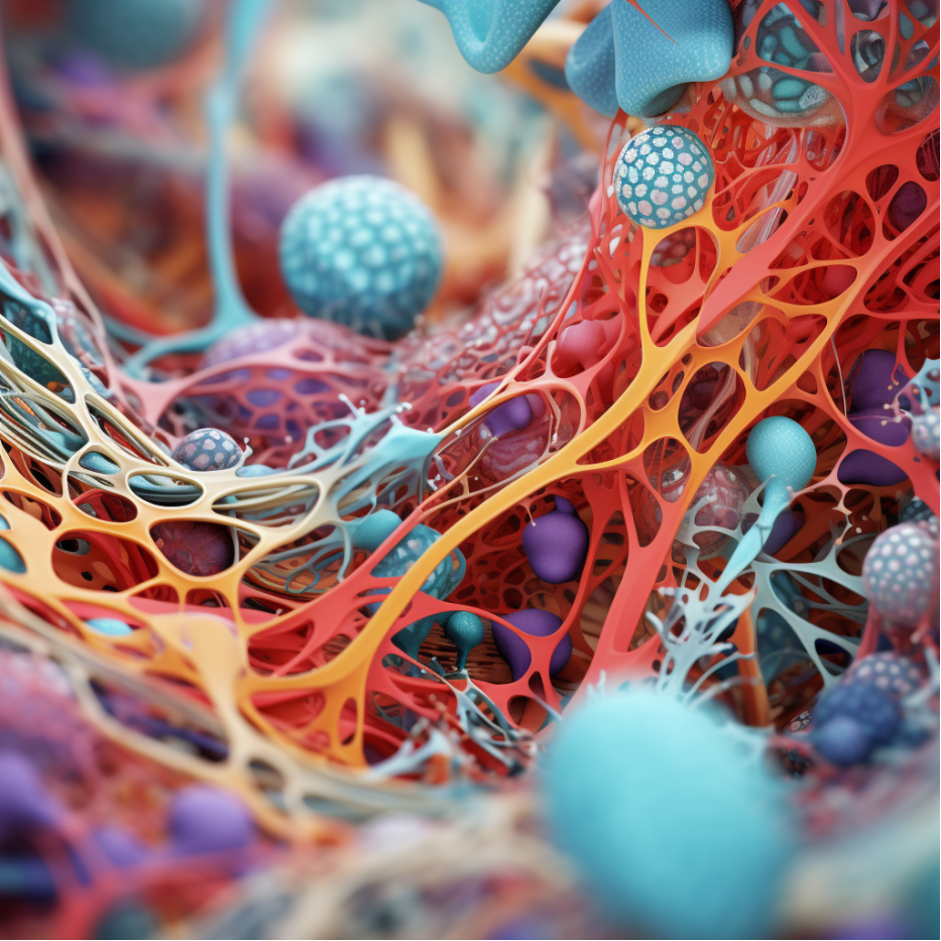
The first stage of rheumatoid arthritis, also known as the early stage, is marked by inflammation of the synovium – the protective sheath surrounding our joints. At this stage, patients may experience mild discomfort, but explicit symptoms may not yet have surfaced [2]. Common symptoms can include fatigue, general malaise, and minor joint discomfort. Although radiographic tests may not show any damage at this point, it is crucial to seek medical attention at the earliest sign of these symptoms. Early detection can significantly influence the progression and management of RA.
Statistics: In the early stage of rheumatoid arthritis, most patients may not exhibit explicit symptoms. However, about 60% of people who do not receive treatment within the first two years of onset tend to have at least one form of disability, highlighting the significance of early diagnosis and treatment. [Source: Scott DL, Wolfe F, Huizinga TW. Rheumatoid arthritis. Lancet. 2010 Sep 25;376(9746):1094-108. doi: 10.1016/S0140-6736(10)60826-4. PMID: 20870100.]
Stage 2: Moderate Stage
During the moderate stage, the inflammation in the synovium intensifies, leading to the thickening of this protective layer. This ongoing inflammation may start to damage the cartilage (the cushioning layer between joints) and bones, causing the typical symptoms associated with RA: swelling, pain, and joint stiffness [3]. These symptoms are often more pronounced in the mornings or after extended periods of inactivity. Mobility may be affected during this stage, but there is generally no severe joint deformity.
Statistics: The moderate stage, where symptoms such as pain, swelling, and joint stiffness start to manifest, affects approximately 35% of RA patients within five years of diagnosis, given the absence of effective treatment strategies. [Source: American College of Rheumatology. (2023). The State of Rheumatology: 2023 Report.]
Stage 3: Severe Stage
The severe stage of RA is characterized by the continued loss of cartilage, leading to decreased joint movement. The persistent inflammation destroys the bone, causing erosions visible on X-rays [4]. At this point, the symptoms become more intense, and individuals may experience significant discomfort and difficulty performing everyday tasks due to joint deformities. This stage necessitates more aggressive treatments, including stronger medications and possibly surgery.
Statistics: The severe stage, characterized by bone erosions and decreased joint movement, is reported in 20-30% of untreated RA patients within ten years of onset [Source: Singh JA, Saag KG, Bridges SL Jr, et al. (2016). 2015 American College of Rheumatology Guideline for the Treatment of Rheumatoid Arthritis. Arthritis Rheumatol. 68(1):1-26.]

Stage 4: Terminal Stage
The terminal stage of rheumatoid arthritis is the most severe. The inflammatory process ceases at this phase, but the damage done to the joints cannot be reversed. The joints may become deformed and fused, resulting in loss of mobility and function [5]. Pain management, physiotherapy, and assistive devices are critical to helping patients maintain as much independence as possible.
Statistics: The terminal stage of rheumatoid arthritis typically occurs after several years or even decades of the disease. The inflammatory process may stop, but the joints’ function could be significantly impaired or lost. The proportion of RA patients reaching this stage has significantly decreased in recent decades due to improved therapeutic approaches [Source: ACR, 2023.]
Understanding RA and Its Treatment
As daunting as these stages may sound, remember that rheumatoid arthritis is a highly individual disease – the progression and intensity of symptoms vary widely among patients. Furthermore, medical advancements have come a long way in managing RA. Modern treatments such as disease-modifying antirheumatic drugs (DMARDs), biological agents, and targeted therapies can significantly slow disease progression, reduce inflammation, and help patients maintain their quality of life [6].
According to a 2023 report by the American College of Rheumatology, early intervention and treatment adaptation in response to disease progression have resulted in improved disease outcomes for many patients [7]. Although there is no cure for RA, these treatment strategies aim to induce disease remission or low disease activity, minimizing joint damage, and preserving function and mobility.
Living With RA
Living with rheumatoid arthritis requires a multifaceted approach involving medication, regular physical activity, balanced nutrition, and stress management. Patient education programs, support groups, and psychological counseling can help patients cope with the emotional burden of RA. Ensuring you have a strong support system, be it medical professionals or loved ones, can make a substantial difference in your journey with RA.
In conclusion, understanding the stages of rheumatoid arthritis and the associated symptoms can help patients navigate their treatment journey more effectively. With early detection, individualized treatment plans, and comprehensive care, patients can lead meaningful and productive lives, despite this challenging disease.
References:
- Arthritis Foundation. (2023). Arthritis by the numbers: Book of trusted facts & figures. https://www.arthritis.org/
- Firestein GS. (2021). Rheumatoid arthritis: Etiology and pathogenesis of rheumatoid arthritis. UpToDate.
- McInnes IB, Schett G. (2017). Pathogenetic insights from the treatment of rheumatoid arthritis. Lancet. 389(10086):2328-2337.
- Aletaha D, Smolen JS. (2018). Diagnosis and Management of Rheumatoid Arthritis: A Review. JAMA. 320(13):1360-1372.
- Singh JA, Saag KG, Bridges SL Jr, et al. (2016). 2015 American College of Rheumatology Guideline for the Treatment of Rheumatoid Arthritis. Arthritis Rheumatol. 68(1):1-26.
- Smolen JS, Landewé RBM, Bijlsma JWJ, et al. (2020). EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis. 79(6):685-699.
- American College of Rheumatology. (2023). The State of Rheumatology: 2023 Report. https://www.rheumatology.org/





