What Is Usually the First Sign of Glaucoma?

Today, we’re unpacking the silent and often overlooked subject of glaucoma—the eye condition that you don’t know you have until, well, you might lose your vision. This condition is one of the leading causes of irreversible blindness, but the kicker? It’s mostly preventable if caught early. please share your experiences at the end.
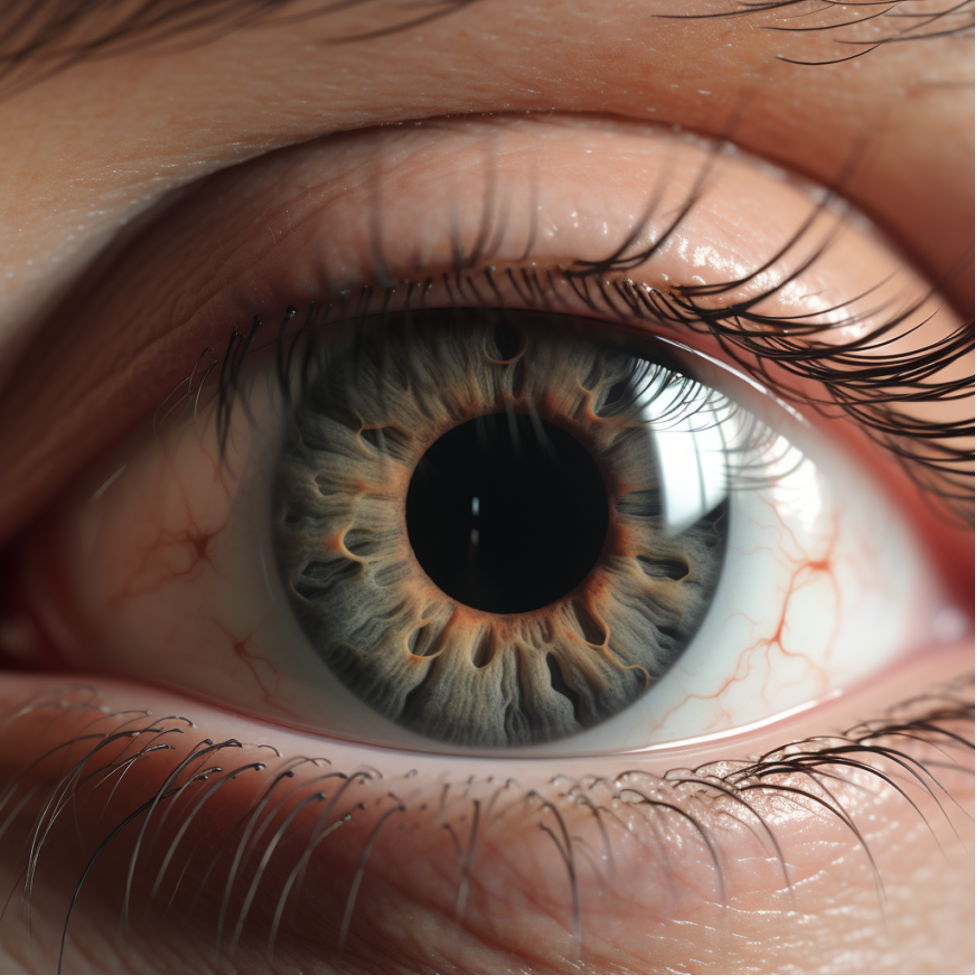
What Is Glaucoma?
Glaucoma is not just a single eye condition; it’s actually a group of eye diseases that affect your optic nerve, leading to potential vision loss or even blindness. This nerve is essentially your highway to seeing the world; it sends visual information from your eye to your brain. Think of it as the Wi-Fi of your visual system. Once it’s damaged, you’re looking at a serious disruption in your visual reception, which could lead to significant vision loss if not treated.
Statistics:
- According to the World Health Organization, glaucoma affects over 76 million people worldwide.
- It’s the second leading cause of blindness after cataracts.
- 10% of those with glaucoma who receive proper treatment still experience loss of vision.
Glaucoma Signs
When it comes to the signs of glaucoma, it’s often like a ninja sneaking up on you—silent, stealthy, and you don’t know it’s there until it’s too late. This is especially true for the most common type, open-angle glaucoma, where the initial symptoms are usually so subtle that they’re easy to miss. It starts with the gradual loss of peripheral vision, which may not even be noticeable in day-to-day activities. You might only discover it when both eyes have been affected, and by then, irreversible damage could have already occurred.
Then there’s angle-closure glaucoma, which is the polar opposite. This type announces its presence with bells and whistles—sudden eye pain, severe headaches, nausea, and sometimes even vomiting. You might see halos around lights and experience a dramatic decline in your ability to see in low-light conditions. It’s like the fire alarm of glaucoma types, requiring immediate medical attention.
Statistics:
- About 50% of people with glaucoma don’t know they have it.
- Symptoms include eye pain, blurred vision, and “halos” around lights.
Causes of Glaucoma
Understanding the causes of glaucoma can be a bit like solving a mystery. While the most common factor associated with glaucoma is elevated intraocular pressure (IOP)—that’s the pressure inside your eyes—this isn’t the whole story. So, let’s dig into some of the leading suspects behind this condition:
- High Intraocular Pressure: Elevated eye pressure is the most frequently cited cause, but not everyone with high IOP develops glaucoma. Conversely, people with ‘normal’ eye pressure can still develop the condition, particularly normal-tension glaucoma.
- Genetics and Family History: Got relatives with glaucoma? Your chances of getting it are higher. A family history of glaucoma can increase your risk by 4 to 9 times, making those regular family get-togethers a good time to discuss eye health.
- Age: Being 60 or older places you at higher risk, and if you’re African American, the risk increases even earlier, from around age 40.
- Ethnic Background: People of African, Hispanic, and Asian descent are at a higher risk compared to Caucasians.
- Medical Conditions: Diabetes, hypertension, and heart disease can increase your risk. Even nearsightedness and farsightedness have been associated with glaucoma.
- Eye Anatomy: Features like thinner corneas and sensitive optic nerves can make you more susceptible.
- Prolonged Medication: Using corticosteroids, especially in the form of eye drops, can elevate eye pressure and thereby contribute to the onset of glaucoma.
- Trauma or Injury: A severe eye injury can trigger glaucoma, either immediately post-injury or years down the line.
Statistics:
- Around 2% of people over the age of 40 have glaucoma.
- Family history can increase your risk by 4 to 9 times.
Quick Poll
How to Treat Glaucoma
Treatment for glaucoma is all about damage control—limiting further damage to the optic nerve and preventing additional vision loss. Unfortunately, any vision loss already incurred is usually irreversible. Here’s a closer look at the various treatment avenues:
- Eye Drops: The most common initial treatment, prescribed eye drops, aim to lower intraocular pressure. These come in various types, like prostaglandins, beta-blockers, and alpha agonists, each with its own benefits and side effects. It’s crucial to use them exactly as prescribed for maximum efficacy.
- Oral Medications: In some instances, oral medications like carbonic anhydrase inhibitors can be prescribed alongside eye drops to manage more severe cases of elevated eye pressure.
- Laser Treatment: In moderate cases or when medications aren’t as effective, laser trabeculoplasty may be advised. This procedure helps improve the eye’s drainage system, thereby reducing intraocular pressure.
- Surgery: In advanced cases or when other treatments fail, surgical intervention becomes necessary. The most common is trabeculectomy, which creates a new drainage pathway for the eye fluid.
- Drainage Implants: Another surgical option is to implant a microscopic drainage tube in the eye to help divert fluid and reduce pressure. These are usually reserved for severe cases or younger patients.
- MIGS (Minimally Invasive Glaucoma Surgery): A newer line of treatment, MIGS offers less invasive options that typically have fewer complications. However, they may not be as effective for advanced glaucoma.
- Complementary Therapies: While not a primary treatment, certain lifestyle changes like a balanced diet and regular exercise have been shown to contribute to lower intraocular pressure.
Statistics:
- 75% of glaucoma can be treated with eye drops.
- 20% of cases might require surgery.
Prevention of Glaucoma
Prevention is always better than cure, but when it comes to glaucoma, outright prevention can be a tricky proposition. You can’t change your genetic makeup or age, but there are steps you can take to manage your risk factors and possibly slow down the progression of the disease. Here’s how:
- Regular Eye Exams: This one can’t be stressed enough. Routine eye screenings are the cornerstone of glaucoma prevention, especially if you’re over 40 or have a family history of the disease. Your optometrist can track subtle changes in eye pressure and the optic nerve over time.
- Control Underlying Conditions: Diseases like diabetes and hypertension are risk factors for glaucoma. Properly managing these conditions can help you keep glaucoma at bay or slow its progression.
- Physical Exercise: Studies suggest that moderate, regular exercise like jogging or walking can help lower intraocular pressure, but extreme sports that involve head-down positions can increase it. A balanced approach is key.
- Healthy Diet: A balanced diet rich in fruits, leafy greens, and fish is not just good for your heart; it’s also beneficial for your eyes. Some studies have shown that foods rich in antioxidants and omega-3 fatty acids can support eye health.
- Limit Caffeine and Fluid Intake: Excessive caffeine can temporarily spike intraocular pressure. Also, drinking large amounts of fluid quickly can similarly elevate eye pressure.
- No Smoking: This one’s a no-brainer. Smoking is detrimental to overall health and can exacerbate a variety of eye conditions, including glaucoma.
- Use Eye Protection: Safety goggles aren’t just a fashion statement when doing activities that could result in eye injury. Trauma to the eye can trigger glaucoma, so it’s best to shield those peepers.
Statistics:
- Routine eye exams can decrease the risk of vision loss by 85%.
- A diet rich in leafy greens can reduce the risk by 20%.
PLEASE SHARE YOUR EXPERIENCE AND THE COMMENTS BELOW SO WE CAN HELP EACH OTHER WITH THE KNOWLEDGE YOU HAVE GAINED.
References:
- World Health Organization. (2021). “Glaucoma: Key Facts.”
- American Academy of Ophthalmology. (2022). “What Is Glaucoma?”
- National Eye Institute. (2020). “Glaucoma, Open-angle.”
- Mayo Clinic. (2021). “Glaucoma: Symptoms and Causes.” Glaucoma Research Foundation. (2022). “Types of Glaucoma.”





