How psychologists are helping children who have lost caregivers to COVID-19

By Amy Edgar

More than 1.5 million children have lost a caregiver during the COVID-19 pandemic, and many of them have suffered these types of traumatic experiences.
While losing a parent or caregiver is always a challenge to a child’s mental health, these traumas are magnified in a situation like COVID-19. A study published by The Lancet and led by epidemiologist Susan Hillis, PhD, who served on the Centers for Disease Control and Prevention’s COVID-19 International Task Force, called such orphanhood a “hidden pandemic” and pointed to the likelihood of the tragic reverberations being felt well past childhood
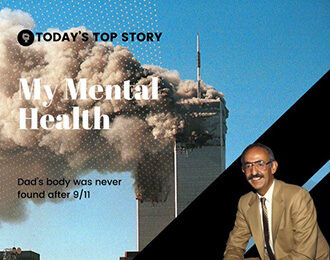
Losing a parent to COVID-19
A child may have a wide range of reactions to the loss of a parent or loved one; grief is a difficult journey. “However, when that loss or death is experienced as a traumatic loss, it can derail development,” said Megan Goslin, PhD, a clinical psychologist, and associate research scientist at Yale University’s Child Study Center.
Goslin’s work focuses on therapeutic interventions with children and families following potentially traumatic events. “Children can develop post-traumatic symptoms that are over and above the normal grieving process,” she said. “Post-traumatic symptoms can greatly lengthen the mourning process. They can also prevent children from focusing on everyday things, like learning math or making friendships.”
Corinn Elmore, PhD, a pediatric psychologist who works with families through Walter Reed National Military Medical Center in Bethesda, Maryland, said that during the pandemic she observed that many of her regular patients without previous anxiety began to experience it for the first time. She also said that her patients who already suffered from anxiety started suffering much more acutely.
Children’s grief during the pandemic is complicated grief, said Julian Ford PhD, ABPP, a professor of psychiatry and law and director of the Center for Treatment of Developmental Trauma Disorders at the University of Connecticut. He noted that “the isolation and loneliness many experienced due to pandemic restrictions made it harder for children to feel the support of close friendships or the comfort of additional caregivers (such as extended family), other sources of support (such as teachers or religious leaders), and even the support of the dying parent (who may be quarantining at home or in the hospital).”
“Another common thing I observed during the pandemic was my pediatric patients witnessing their parents losing their parents to COVID,” Elmore said. “While the children grieved for these lost grandparents, they also wondered if they might lose their parents, too.”
Carla Stover, PhD, an associate professor at the Yale Child Study Center, researches the impact of violence and trauma on child development. The “overarching stress” of everyone living through the pandemic and the heightened levels of continued anxiety can make treating patients a different experience, according to Stover. She points to pandemic stressors that even children who have not lost a caregiver may face, such as difficulty navigating friendships with families who are not vaccinated or experiencing stress from overhearing unsettling pandemic news or discussions.
For children who are experiencing devastating grief due to COVID deaths, these stressors can be far worse. “The uncertainty about who will contract COVID and who will become very ill adds further anxiety for the child, who may fear the loss of others [the other parent, other family, friends] and contracting COVID themselves,” said Ford.
Successful approaches to children’s grief
With the shift toward telehealth at the beginning of the pandemic, many providers weren’t sure at first if they could succeed in delivering their usual standard of care, Stover noted. But given the need—especially for children going through intense grieving— “we had to learn to deliver therapy in new ways,” she said. She explained that providers managed to adapt and learned to do things such as make better use of technology with such strategies as screen sharing or dropping off props for play-based therapy at people’s homes so that parallel play could happen virtually.
For children who had lost caregivers or other loved ones to COVID-19 or whose parents were sick with COVID, Elmore counseled the use of transitional objects, since spending time with the sick or dying parent wasn’t an option. Among the activities she recommended to children were writing a letter or creating a drawing to be delivered to their loved one, or simply keeping a favorite photo of the loved one nearby.
In general, Elmore found that virtual therapy sessions required her to change her approach, and, overall, she said she had to spend a greater percentage of time empowering parents. She found that because kids under 9 years old had trouble focusing for long periods of time, she would spend about 80% (rather than her usual 30%) of a session with the parent alone. For 9- to 12-year-olds, it was about 50/50 child and parent. With patients over 13 years old, she didn’t find much of a difference between in-person and virtual sessions. “I worked to teach parents how to counsel a child through grief, including some of the techniques I would normally have used with a pediatric patient myself in the office,” Elmore said. “Together, the parent and I would work on a narrative for the child.”
Stover added that while there have been some negatives in delivering virtual care, such as a lack of privacy in some living situations and unequal access to broadband internet service, they were greatly outweighed by the positives: reaching more parents and families by meeting people where they are and when they are available.
For example, for parents widowed by COVID-19, setting up childcare for other children while one is in a session can be an insurmountable financial burden on top of counseling fees. With in-home teletherapy, this can become a nonissue, said Goslin. Virtual visits can also provide an opportunity to speak to the surviving caregiver and children more easily either together or apart.
“For all children and families in need of therapy, virtual therapy has particularly been helpful in engaging dads,” said Stover. She anticipates that virtual visits are here to stay; even with some patients choosing to return to in-person appointments, others may find it more convenient to stay virtual.
Psychologists working with families who are seeking additional information after losing a caregiver to COVID-19 might refer them to helpful resources such as the CDC’s COVID-19 Parental Resources Kit, the National Child Traumatic Stress Network, or the Yale Child Study Center. Focusing on the mental health of the children is an obvious priority, but it isn’t the only one, Ford said. “Providers need to consider not only the emotional needs of the bereaved child but also those of their caregivers, who need to be supported in their own grieving so that they feel competent and successful in providing for their children.”
Long-lasting effects
According to the Lancet study, children orphaned by COVID-19 “often face adverse consequences, including poverty, abuse, and institutionalization.” For children who don’t get the mental health care they need to weather the loss of a caregiver, the results can mean lifelong struggles and addictions, according to Nora Volkow, MD, director of the National Institute on Drug Abuse.
Psychologists play a major role in the welfare of these children. “Though the trauma a child experiences after the loss of a parent or caregiver can be devastating, there are evidence-based interventions that can prevent further adverse consequences, such as substance use, and we must ensure that children have access to these interventions,” said Volkow.
The impact on BIPOC children
There have been a greater number of caregivers lost to COVID-19 in BIPOC communities. Researchers recently found that “Black children are disproportionately affected, comprising only 14% of children in the United States but 20% of those losing a parent to COVID-19”.
Goslin noted that she has seen this national statistic play out locally among the many families that she works with in New Haven, Connecticut (including among Black patients and other people of color, immigrants, essential workers, and more). “I’ve observed them being disproportionately impacted by all the stresses and strains of COVID,” said Goslin. “Working from home is not an option for everyone.”
What next?
What’s needed for all populations is the allocation of more resources for early identification and treatment of mental health issues. “The mental health care system was stretched thin even before the pandemic,” said Goslin. Early treatment can not only be more effective for mental health; it can also be more cost-effective in the long run.
Ford agrees and notes that economic support is a crucial component of supporting grieving children. “The pandemic has highlighted the need for funding for universal pre-K and childcare for younger children and economic support for families with children,” he said. For children who have lost a caregiver, this support could be a lifeline to basic necessities so that they and their remaining caregiver can focus on emotional healing.
Lucie Cluver, PhD, a coauthor of the Lancet study and a professor of child and family social work at Oxford University and an honorary professor in psychiatry and mental health at the University of Cape Town, said, “We have strong evidence from HIV and Ebola to guide solutions. We need to support extended families or foster families to care for children, with cost-effective economic strengthening, parenting programs, and school access. We need to vaccinate caregivers of children—especially grandparent caregivers” Cluver also underscored the real urgency of this situation: “We need to respond fast because every 12 seconds a child loses their caregiver to COVID-19.”