Confronting My Caregiving-Related Trauma

Nicole Dauz
May 2021
At the beginning of my caregiver journey, I resisted making the association between my new role and the mental health issues I was experiencing. These included excessive worrying about my daughter’s safety and my body breaking out in rashes.
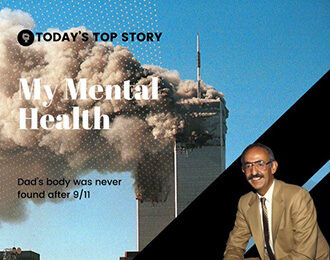
I associated trauma (and the PTSD that follows) with victims of abuse and veterans. Maybe part of that was due to the increased media coverage in a post-9/11 world around military families advocating for resources to support men and women returning home with PTSD.
I did not equate learning that my child had a global development delay with the trauma I now realize I carried with me in the years following her diagnosis. Even though my daughter would require weekly therapy at 18 months–physical therapy to learn how to walk and occupational therapy to learn how to hold a spoon and put on socks–it was in no way comparable to being assaulted or experiencing combat. Or at least that’s how I rationalized it.
This is one example of how we unknowingly compare ourselves and our situations with others and how this habit can be so very detrimental to our own healing journey.
Two things happened that changed my perspective about the connection between caregiving and trauma. First, I distinctly remember a close friend telling me–which shocked me at the time, “Nicole, you experienced trauma with Summer.” Secondly, I started to realize that I was in a constant “on” state while in the house. My mind and heart would always be racing and wondering Where is Summer? And What is she doing?
When I was at work, I didn’t experience those types of thoughts. At work, I was able to go to the bathroom by myself and eat my lunch in peace. (It’s fair to say this was my little slice of heaven.) This awareness of my racing thoughts was most noticeable when I would go on my annual adults-only trip down south for a week. I could literally feel my body decompressing and my mind relaxing. It was only then that I was able to rest, rejuvenate, and sleep soundly.
It would usually take a few days for me to fully unwind–for my brain to know that it was safe to relax completely. I was always amazed at how much I could sleep while I was away. Both afternoon naps on the beach and a solid eight to nine hours at night.
Is this what researchers are referring to when they talk about the fight or flight response and the impact that it has? I imagine that you know exactly what I’m referring to–that stressful situation that makes the heart pound, the breath quicken, and the muscles tense up.
The American Psychological Association published an article that explains how long-term stress effects all systems of the body called Stress effects on the body. The article goes in depth of how staying in fight or flight for long periods of time (aka chronic stress) impacts 7 different systems within the body.
Now I think of how much that denial prevented me from seeking solutions earlier on in my caregiver journey. It’s never about the label itself, it’s about finding the tools, strategies, and supports to help you heal, find acceptance, and live a meaningful life. Here are some tactics that can help us process our caregiving-related traumas and protect our mental health through periods of prolonged stress:
- Reach out for help. Confiding in even one person helps move us from denial to acceptance.
- Find community so we know that we’re not alone.
- Do something for ourselves that brings us joy.
Remember: Just because we have experienced trauma in our lives, it doesn’t mean that it has to define us. That’s why I’m so passionate about caregiver self-care. Learning the tools and strategies to take care of ourselves is the first step in the healing.
Please comment below or contact me at nicole@nicoledauz.com to learn more about how I can help you shift from feelings of overwhelm and stress to feeling of gratitude and joy.