Why There’s New Hope for Alzheimer’s Patients
by Allysia Finley
The Wall Street Journal updated December 2021
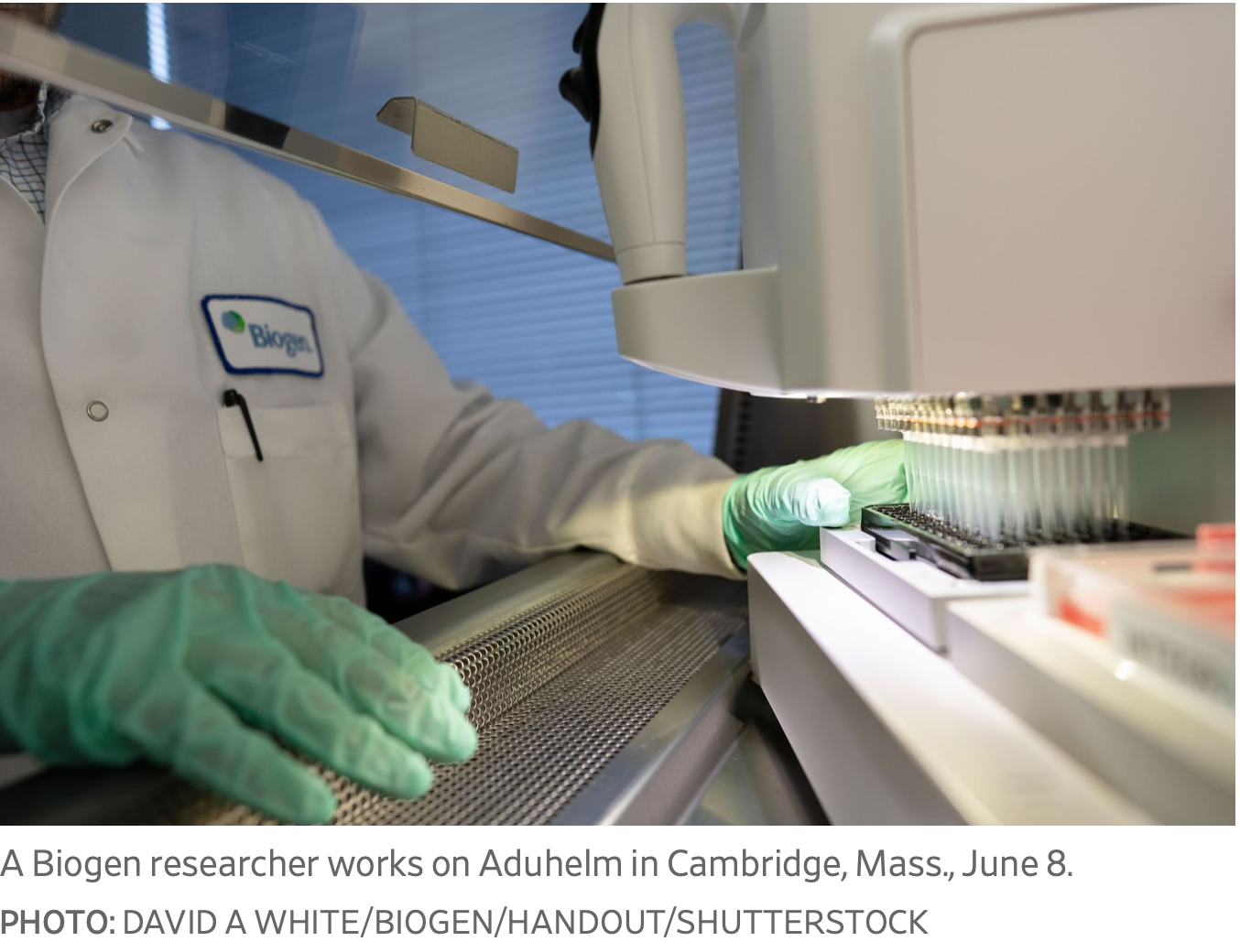
Biogen’s aducanumab isn’t a cure, but the trials were promising—and other therapies are in the works.
How much hope can Alzheimer’s patients and their loved ones take from the Food and Drug Administration’s approval of a new drug this month? Researchers and drug makers have labored fruitlessly for decades to develop treatments that can slow the disease’s progression. More than 100 experimental drugs have failed in clinical trials, but researchers may be on the cusp of a breakthrough.
Biogen’s newly approved monoclonal antibody drug, aducanumab (known by the brand name, Aduhelm), is the first treatment that has shown evidence in clinical trials of reducing amyloid plaque in the brain and slowing cognitive decline. It isn’t a cure. But it and similar treatments could transform the disease from a death sentence to a manageable condition like diabetes or multiple sclerosis. “We are now about to take the journey toward transforming Alzheimer’s disease from a terminal disease as we know it to a chronic disease,” Cleveland Clinic neurologist Marwan Sabbagh said in a NeurologyLive video cast.
Alzheimer’s is characterized by buildup of amyloid plaque and tangles of tau protein in the brain, which typically begin developing a decade or two before the cognitive symptoms. It isn’t known what causes these plaques and tangles to form. A leading theory has been the “amyloid cascade hypothesis”—that amyloid plaque promotes aggregation of tau tangles, which in turn trigger neuron death and loss of memory and cognitive ability.
Researchers have investigated the possibility that removing amyloid could halt the cascade and preserve brain function. More than 50 drugs aimed at clearing amyloid have failed to show a benefit in clinical trials, leading some researchers to doubt the theory.
The FDA cites several other reasons past Alzheimer’s drug trials might have failed. Some didn’t properly screen participants to ensure they had Alzheimer’s rather than another form of dementia. Some involved patients in the later stages of the disease, when significant and irreversible brain loss has already occurred—too late, perhaps, for the treatment to help.
Enter aducanumab, a monoclonal antibody that binds to amyloid and breaks it up. It was cloned from healthy elderly people who didn’t get Alzheimer’s or had unusually slow cognitive decline. Biogen learned from the mistakes of earlier clinical-trial failures and tested its drug at multiple dosages on early-stage patients. Early results were encouraging, later ones mixed.
Biogen’s initial trial, with 200 patients, showed that higher doses over time increasingly reduced amyloid and slowed cognitive decline—the first Alzheimer’s drug to demonstrate what the FDA describes as a “proof of concept.” But Biogen’s two later trials, each with some 1,600 patients, were muddled. While a high dose cleared 71% of amyloid in 18 months, Biogen stopped the trials early because the drug didn’t seem to slow cognitive decline in the aggregate.
Yet when Biogen later pored over the data, it discovered that results in one trial were very positive. In that trial, patients receiving the highest dosage showed 25% to 28% less decline in problem-solving and memory, respectively, compared with the control group after 18 months. In the other trial, the results showed the drug failed to slow cognitive decline. But in the latter trial, 25% fewer patients in the highest-dose group received 14 doses—the treatment duration that was found in the early phase trial to slow cognitive symptoms—which could explain the lack of benefit.
Notably, patients in both trials who received 14 infusions of the highest dosage showed similarly positive results for amyloid reduction and cognitive decline after 14 months, Dr. Sabbagh and Jeffrey Cummings noted in the Journal of the Alzheimer’s Association last October. Higher doses also reduced the levels of tau tangles, consistent with the amyloid-cascade hypothesis.
Brown University neurologist Stephen Salloway treated more than 60 patients in Biogen’s trials who received aducanumab. At a hearing of an FDA advisory panel last November, Dr. Salloway testified that his patients receiving aducanumab declined less than expected over several years.
He cited the example of a retired school superintendent, now 80 years old, who developed memory loss and trouble expressing himself six years ago. With five years of monthly infusions of high-dose aducanumab, his cognition remained remarkably stable. “He only began to decline after aducanumab was stopped in March of ’19,” Dr. Salloway said. “But he’s doing better now back on aducanumab through the follow-on trial, living at home, driving and socializing regularly with his friends. His positive response to aducanumab was not isolated.”
The outside panel voted against approving the drug because of the messy clinical-trial data. The FDA usually follows the recommendations of outside panels, but it isn’t obliged to—and in this case, it didn’t. The agency granted Biogen “accelerated approval,” which is permitted for medications that “treat serious conditions, and that fill an unmet medical need” based on “a surrogate or intermediate clinical endpoint”—in this case, reduction of amyloid plaque in the brain.
More than 70 Alzheimer’s drugs are in the clinical pipeline, many employing different strategies. Neurologists like Dr. Sabbagh believe that ultimately a combination of therapies will be needed to hold off or—dare to dream—reverse Alzheimer’s. “I think we are now where MS was when I graduated from medical school 29 years ago,” he said.
It was 1993 when the FDA approved the first treatment for multiple sclerosis. Now patients have some two dozen options, which can treat different forms of the disease, significantly slow progression, and reduce flare-ups. The good news is Alzheimer’s research is advancing much faster thanks to advances in technology. Some treatments in the pipeline are aimed at regenerating neurons. The breakthrough may take far less than a generation.