Experts Forecast Cancer Research and Treatment Advances in 2022

The American Association for Cancer Research Jan 5, 2022, by Calley Jones, Ph.D. Updated Feb 11, 2022
The year 2021 defied our expectations in a variety of ways. The delta and omicron COVID-19 variants imposed unprecedented challenges on the health care system and threatened our hopes of an end to the pandemic, but widespread vaccine distribution provided protection, preventing an estimated 36 million cases and 1 million deaths in the United States.
As omicron called into question the efficacy of existing vaccines, tests, and treatments, the U.S. Food and Drug Administration (FDA) provided new options, in the form of emergency use authorizations for the first two oral COVID-19 drugs, nirmatrelvir/ritonavir (Paxlovid) and molnupiravir (Lagevrio).
Aside from the pandemic, supply chain delays and worker shortages sparked frustration, but the national unemployment rate gradually fell to its lowest percentage since February 2020. Through a year of harsh weather conditions ranging from ice storms to wildfires to hurricanes and tornadoes, the United States doubled down on initiatives to battle climate change.
In spite of the year’s setbacks, the field of cancer research also made progress.
The FDA approved 16 new oncology drugs—including two to treat genetic conditions that cause high rates of tumor formation—as well as two cancer detection agents that help physicians better identify certain tumors during imaging or surgery. We celebrated the 50th anniversary of the National Cancer Act, saw marked progress in many areas of cancer research, and helped provide cancer patients with reliable information about their COVID-19 risks and vaccine efficacy.
As in previous years, we have asked a panel of experts to reflect on the progress made in 2021 and forecast their predictions for cancer research in the year 2022. We spoke with AACR President-Elect Lisa Coussens, Ph.D., FAACR, about basic research; AACR board member and co-editor-in-chief of Cancer DiscoveryLuis Diaz Jr., MD, about precision immunotherapy; co-editor-in-chief of Cancer Prevention Research Michael Pollak, MD, and deputy editor of Cancer Prevention Research Avrum Spira, MD, about cancer prevention; and AACR board member and former Annual Meeting Program Chair John Carpten, Ph.D., FAACR, about cancer disparities.
PRIORITIES FOR BASIC RESEARCH IN 2022
“There isn’t a drug on the market that doesn’t have its origins in a basic science discovery,” said Lisa Coussens, Ph.D., FAACR, chair of the department of Cell Development and Cancer Biology at Oregon Health and Science University, when asked about the ways that laboratory science has shaped the landscape of cancer care. “We can’t lose sight of the importance of basic research at any step in the pipeline toward advancing cancer medicine and improving outcomes for our patients.”
Basic science—fundamental research about the way cells and molecules function and interact—spans applications from protein chemistry to cell genomics to animal models. Such discoveries help researchers determine, for example, which proteins can be targeted with drugs to fight a disease, or which biomarkers might help determine a patient’s prognosis or course of treatment.
An important priority for improving our knowledge of cancer cell biology, Coussens explained, is to better understand how cells shift between different states, especially in response to a disease or therapy.
“We need to understand nuances between different tissue states within our body, and how they respond to changes in their environment,” Coussens said, noting that this is true in healthy organs as well as in evolving tumors, where single-cell types typically steer disease processes but are dependent on cues from the multiple cell types surrounding them.
“Understanding those nuances will lead to bigger discoveries about how to target cell state changes so we can return cells back to normal control mechanisms,” she continued. Tumor cells are not the only cells that might change their patterns of gene expression and metabolism during the course of cancer progression and treatment, however. Other cells that surround and interact with the tumor, such as fibroblasts and immune cells, play a vital role in determining how the tumor behaves.
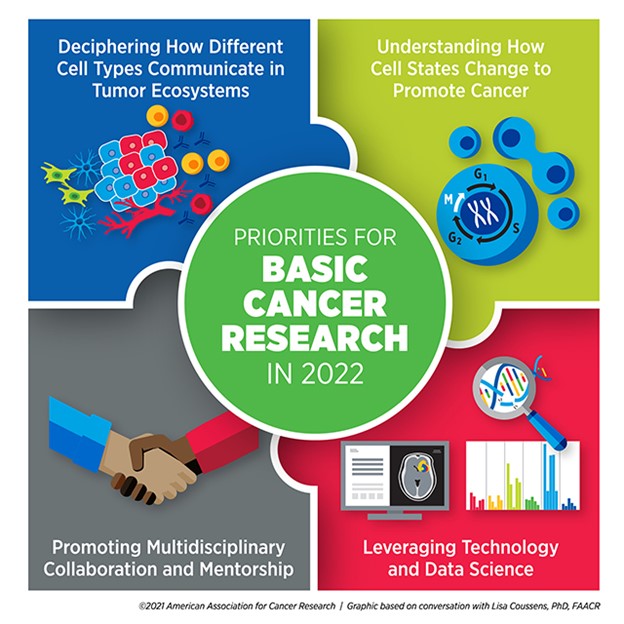
“A full understanding of tumor ecosystems includes the neoplastic cells—the ‘bad guys’ with mutations—as well as the normal host cells that are recruited or co-opted to help tumor cells survive and disseminate,” Coussens said.
Emerging classes of therapies, such as immune checkpoint inhibitors, leverage elements of the tumor microenvironment to kill cancer cells. In order to develop more drugs targeting these cancer support systems, researchers need to learn more about how tumors interact with their surroundings.
“I think the next years will bring a major focus on understanding communication networks between all the different types of cells in tumor ecosystems,” Coussens said, adding that a basic understanding of cell communications could produce benefits beyond the scope of cancer. “Basic discoveries about tumor ecosystems can have far-reaching impacts on autoimmune diseases, chronic inflammatory diseases, and how individuals respond to therapies that are designed to treat Alzheimer’s, for example,” she explained.
Coussens believes that many of these discoveries will be driven by the expanded use of technology and data science. Since the turn of the century, rapid advances in genomics, proteomics, and metabolomics have created an abundance of biological data from patients, animal models, and cell lines. Designing computational programs capable of integrating these data and determining how to analyze them in meaningful ways has been a constant source of innovation over the past 20 years.
Coussens emphasized that continued progress in this area could significantly shape basic research in the coming years. “The biggest impact we’re seeing right now is with the emergence of technology development and computational data sciences,” Coussens said. “I think the greatest advances we will see over the next several years will be emerging out of team science embracing technology, data science, and biology.”
As technological advances spur more integration between different disciplines, Coussens predicts that collaboration will become more crucial than ever. “Science has changed—we no longer do science in isolation,” she said. “The best science today, I think, comes out of multidisciplinary team science. I’m a biologist, but I now need to be able to communicate with data scientists, epidemiologists, and chemists.”
Coussens expressed that young investigators entering the field should consider this new paradigm when planning their training. “The more you can round out your education in a multidisciplinary way, the better. You need to be able to communicate your science with people who don’t necessarily speak your field’s language.”
Part of her advice hinged on trainees finding strong mentors who can help guide them toward these opportunities, especially as they recover from lost time and funding resulting from the COVID-19 pandemic. “Invest your time and energy in identifying mentors who care about who you are and the trajectory of your career. Find mentors who you will grow to respect and love,” she said.
Overall, Coussens was optimistic about the state of basic research moving forward.
“The basic science discoveries we’re going to see in the next five years will reshape the medical landscape for years to come,” she said.
PRIORITIES FOR PRECISION IMMUNOTHERAPY IN 2022
The art of deciding which cancer therapies to give a patient, based on their individual tumor characteristics, has evolved over the past several decades, according to Luis Diaz Jr., MD, head of Solid Tumor Oncology at Memorial Sloan Kettering Cancer Center and a member of the National Cancer Advisory Board. Such decisions were first made based on protein markers expressed by the tumor, then by genetic changes in the tumor’s DNA. Now, Diaz said, a precise understanding of tumor characteristics can predict which patients may benefit most from immunotherapy.
“One example has been PD-L1 overexpression, either on the tumors themselves or on the surrounding cells,” Diaz said. “Another is mismatch repair deficiency, which seems to prime cells to become very sensitive to immunotherapy.”
This is just one of the ways that the fields of precision medicine and immunotherapy have grown to complement each other in recent years. As Diaz noted, antibodies targeting PD-1 or PD-L1 have become an effective therapy for patients whose tumors express these immunosuppressive markers.
The treatment of patients with CAR T cells—immune cells which are harvested from a patient’s body, engineered to target tumors, and returned to the patient’s bloodstream—represents an even more patient-specific approach to immunotherapy.
But these therapies are not appropriate for all cancer types, and many patients who receive these therapies eventually relapse, creating a need for the expansion of immunotherapy types and indications.
Diaz believes researchers can improve the efficacy of immunotherapy by offering it earlier in a patient’s course of treatment.
“In many cases, we’re testing new therapies on patients for whom all standard therapies have already failed,” he said. “As we move forward, we need to begin to treat earlier in the diagnosis,” Diaz emphasized that treating advanced cancer poses far more challenges than intervening in early-stage disease or preventing tumor formation altogether. “If we can begin to bring targeted therapy and immunotherapy into the prevention space, I think we’ll see a profound impact,” he said.
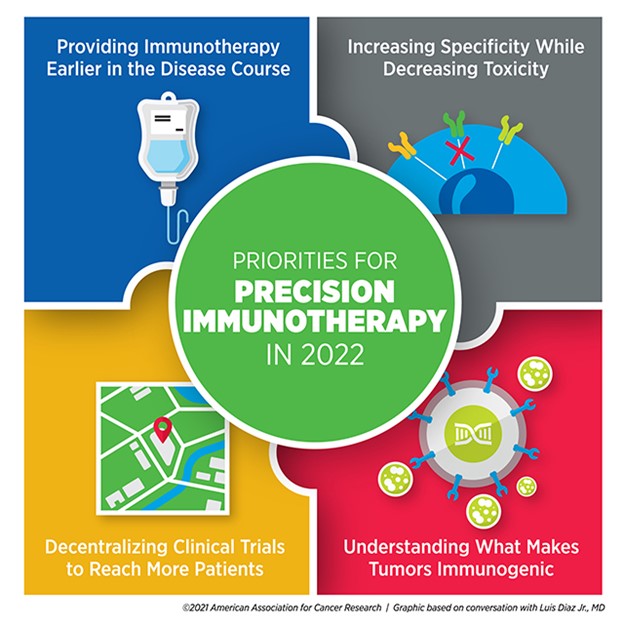
A different approach to improving immunotherapy efficiency is to reach more patients by making cell-based immunotherapies, such as CAR T, effective against a broader range of tumor types, including solid tumors. To overcome these hurdles, Diaz said, “The priority needs to be in maximizing specificity and minimizing toxicity.”
Solid tumors, Diaz explained, are often heterogeneous. An immune response against a single target may kill some of the tumors, but cancer cells that don’t express the target may continue to grow and evade the immune system. Researchers have designed CAR T cells that target multiple tumor cell markers, but more targets also increase the likelihood of harmful side effects. “It’s a mathematical problem we can’t solve very easily,” Diaz said. “We need some clever new ideas.”
Boosting the number of people who receive immunotherapy also involves addressing accessibility issues, especially for patients in rural or under-resourced communities. Diaz speculated that the increase in remote care options resulting from the COVID-19 pandemic might provide a blueprint for the decentralization of clinical trials, paving the way for large cancer centers to collaborate with community hubs.
He emphasized that one way to promote decentralization is to encourage more clinical trial ownership from clinicians rather than pharmaceutical companies. “I’d like to see our investigators becoming the initiators of more trials to be run at large cancer centers and elsewhere,” Diaz said.
He noted that clinical trial decentralization will pose some challenges, such as standardizing procedures and supplies and ensuring that quality does not suffer. However, he was optimistic that it would eventually improve care. “I think it will make clinical development move faster than it ever has before,” he said.
Targeting new populations and tumor types with immunotherapy, however, will only benefit patients whose tumors mount an immune response. Some tumors—deemed immunologically “cold”—expertly evade the immune system, and the mechanisms underlying that process are complex.
“We need a better understanding of what makes tumors immunogenic so we can harness that knowledge to make cancers more immunogenic,” Diaz said. He noted that research into the interface between immune cells and cancer cells has done a great job of producing the therapies on the market today, but that advancing precision immunotherapy will require those efforts to continue.
“As exciting as everything is that we’re doing, we need to do so much more,” Diaz said. “What’s popular right now is probably only the tip of the iceberg.”
PRIORITIES FOR CANCER PREVENTION IN 2022
“The most transformative impact we could have on cancer care would be to prevent cancer from happening in the first place,” said Avrum Spira, MD, a professor of medicine, pathology and laboratory medicine, and bioinformatics at the Boston University School of Medicine and global head of the Lung Cancer Initiative at Johnson & Johnson.
Spira and his colleagues study how physicians can better detect early-stage lung cancer or signs of precancerous changes in the lungs. He also studies how to intervene in these early stages to prevent disease progression.
“Researchers have found molecular alterations in late-stage cancer and used that information to develop new targeted therapies and immunotherapies that are transforming the treatment of advanced-stage disease,” Spira said. “It’s absolutely critical to moving that fundamental molecular understanding to early-stage and even premalignant disease.”
Understanding what drives benign cells into a tumorigenic state is an important component of this process, Spira emphasized. Drawing on the success of large-scale programs such as The Cancer Genome Atlas, the Human Cell Atlas, and the Human Tumor Atlas Network, dedicated to fully characterizing the blueprints of the human body, researchers have embarked on the development of a Pre-cancer Atlas.
“Within the Human Tumor Atlas Network, researchers are forming large coalitions for multiple different cancer types to develop a temporal and spatial atlas of the cellular and molecular changes associated with the transition of a premalignant lesion to a full-blown invasive cancer,” Spira said. “I think, in 2022, we’re going to see a proliferation of those types of studies, generating a vast amount of cellular and molecular data from premalignant tissue across many cancer types.”

Spira believes such an atlas will benefit patients in two key ways: the development of biomarkers that can help predict which precancerous lesions will advance to cancer, and the identification of drug targets to stop the progression.
“For most cancer types, we don’t know what those early events are, and therefore, we have no effective way to intercept the disease process,” he said. “I think in 2022, we will begin to understand these events and gain unprecedented insight into targeted approaches aimed at intercepting premalignancy.”
Spira elaborated more on the need for biomarkers, which may not only identify patients at an elevated cancer risk but may also determine which patients with abnormal imaging results may need a biopsy. The most effective biomarkers, he stressed, would be the ones detectable via noninvasive tests.
“I’m excited about the future of blood-based tests looking at nucleic acids,” Spira said. “The technologies are evolving very rapidly to the point where they can now detect very small amounts of DNA or epigenetic changes that are circulating in the blood, and they can screen people across multiple cancer types.”
While blood-based liquid biopsies have attracted a great deal of attention in recent years, Spira also drew attention to other emerging noninvasive tests with the potential to have a significant impact on early cancer detection, such as urine markers of urologic cancer, stool markers of colon cancer, and nasal brushings to assess lung cancer risk.
Spira hopes these noninvasive tests can be integrated with each other and with imaging results to give the best possible assessment of a patient’s risk. “That’s a complicated space, but I think this convergent approach is one that will advance significantly in 2022,” he said.
Even noninvasive tests, however, can only benefit patients who are able to access them. Spira pointed out a few ways the field adapted during the COVID-19 pandemic that could continue to be leveraged moving forward.
“We need to find ways to get screening to patients as opposed to them having to come to the hospital,” Spira said. He highlighted advances such as remote clinical trial management, as well as mobile CT and radiology units, set up in large vans or trucks that can drive to various neighborhoods to perform screening. Used during COVID-19 to promote social distancing and minimize virus exposure, such units could be used in the future to help people catch up on screenings missed during the pandemic, especially in areas with poor health care access.
Spira also noted that the pandemic placed a spotlight on behavioral risk factors that increased COVID-19 susceptibility and the risk for severe diseases, such as smoking, alcohol consumption, obesity, and physical inactivity. He pointed out that, often, these same behaviors contribute to cancer risk.
“This has become a teachable moment,” Spira said. “I think we can encourage the public to alter some cancer-causing behaviors that are also related to virus susceptibility.”
Michael Pollak, MD, a professor of oncology and medicine at McGill University in Montreal, Canada, who studies cancer prevention through the lens of reducing risk, also emphasized addressing lifestyle behaviors that affect multiple health conditions.
“An important trend for 2022 may be the concept of healthy lifestyle behaviors integrated across diseases,” Pollak said. “We have to recognize that some of the activities and lifestyles and approaches to cancer risk just contribute to overall good health.”
While many behavioral factors are known to broadly increase the risk of several cancers, Pollak noted that risks vary in unique ways among different individuals.
“Oncologists are used to a personalization of treatments,” he said. “We try to find out what treatment would be particularly useful for one patient as compared to their neighbor. In prevention, we may discover an analogy to that customization.”
He explained that an individual assessment of risk may make the message of behavioral intervention more personal. “If you hear your doctor saying that, in your particular case, the way your body is put together, your weight especially increases your risk for cancer, it may help motivate some people.”
Pollak believes risk assessment can be further personalized beyond the level of the individual, down to the level of discrete cell types. “We’re used to thinking of a person’s cancer risk as if the person was homogeneous, but carcinogenesis takes place at the cellular level,” he said. “We need to know what’s going on differently in the different cells that might determine risk on a per-cell basis.”
Pollak mentioned the Pre-cancer Atlas as an important vehicle for realizing this goal. “With the Pre-cancer Atlas, we’ll learn more about the cellular composition and subcellular features that lead to carcinogenesis,” he said, noting that such a granular understanding of tumor formation could pave the way for improved therapies.
“We really won’t be able to prevent every cancer, but even if we confine our goals to preventing the subset of cancers that are preventable, that’s estimated to be about half of all cancers,” Pollak concluded. “Even acknowledging the limitations, the potential gains are absolutely enormous.”
PRIORITIES FOR CANCER DISPARITIES IN 2022
The past two years have presented health care challenges beyond COVID-19, encompassing financial and access-related struggles that affected many facets of medicine, including cancer care. Many individuals have had to delay routine cancer screenings, alter the course of treatment, or miss follow-up appointments as a result of the pandemic. Such problems were more pronounced in some communities than others.
“The pandemic has definitely impacted our opportunities to move forward toward eliminating disparities in all areas of cancer research,” said John Carpten, Ph.D., FAACR, chair of the Department of Translational Genomics at the University of Southern California Keck School of Medicine and chair of the National Cancer Advisory Board. “As we consider gaps in cancer screening and cancer diagnosis, many challenges were further exacerbated in underrepresented minority communities during the pandemic.”
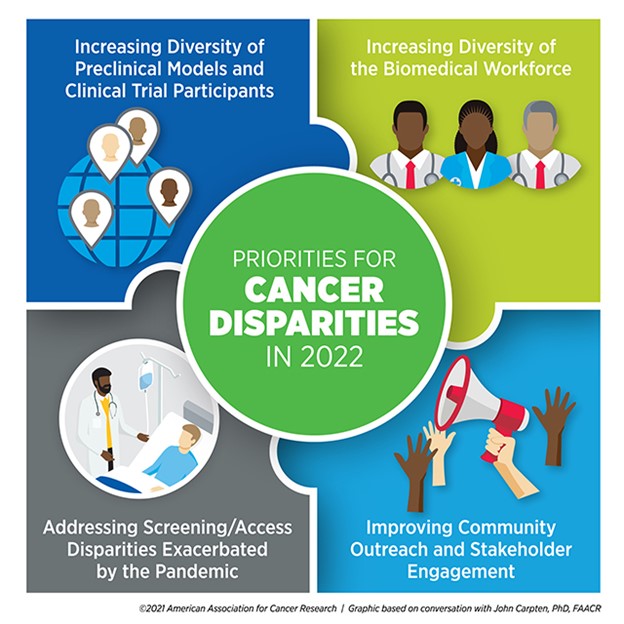
Carpten also pointed out the disproportionate challenges minority cancer researchers faced during COVID-19. “Many underrepresented minority investigators, who may have already had challenges in terms of access to funding, were also impacted severely by the pandemic,” he said. “This is especially true for early-stage investigators and postdoctoral fellows who were unable to be in their laboratories to perform research.”
Although the issue of lost time and funding due to the pandemic may be difficult to solve, Carpten believes that other initiatives to support underrepresented minority researchers—especially trainees and early-career investigators—will positively influence health disparities research in 2022.
Carpten specifically listed diversifying the biomedical workforce as a key priority for tackling health disparities. “Increasing underrepresented minority faculty members will increase the number of mentors who will then be able to train more underrepresented minorities and fellows,” he said.
He mentioned the National Institutes of Health (NIH) FIRST program, a funding opportunity provided to institutions to promote the hiring of early-career investigator cohorts from diverse backgrounds in support of their career development. Providing a supportive environment and sufficient resources to these investigators, Carpten said, can make significant strides toward ensuring a successful career trajectory in academic research.
“We believe that this is going to be a huge component in the growth of underrepresented minorities in the area of biomedical research, specifically cancer research,” he said.
Encouraging the diversity of researchers, however, is only one step where meaningful interventions can occur. Another is the broader inclusion of diverse patients and samples in cancer research, especially of patients recruited into clinical trials.
“We need to understand the broader impact of new therapies for all people, preferably prior to approvals, to ensure that we have the most accurate picture relative to effectiveness and toxicity profiles across representative groups of patients,” Carpten said.
Diversity in preclinical studies, including patient-derived samples, genetic data, and model systems, is also key to understanding the biological basis of cancer health disparities. “Whether it’s understanding the influence of genetic factors on cancer risk or understanding how collections of mutations that occur in cancer cells differ across individuals from different groups, it will be very important for us to continue increasing representation of the reagents, models, and data that we use,” Carpten said.
“Ensuring that we understand how biological changes impact cancer initiation, progression, and growth across an array of models will provide additional information so that we can really capture the full complexity of cancer,” he added.
Carpten also encourages working to address the cultural, social, and access-related issues underlying cancer health disparities by striving harder to engage with the community.
“We need to advance our relationships with various stakeholders, especially in terms of community engagement, outreach, and involvement,” Carpten said. “If we don’t build better relationships with the community, get their feedback, understand their issues, and work together to address them, I think we’ll continue to have challenges.”
As observed during the pandemic, improving community engagement can help health care providers build trust with their patients, bring care to broader geographic areas, and better understand the needs of the population’s disparities researchers are working to serve.
“I really look forward to working with my colleagues in academia, industry, and the government, but most importantly, with our colleagues in the community,” Carpten concluded. “Their voice really needs to be heard and will be key in achieving cancer health equity.”